Abstract
Background:
Patients with acute myeloid leukemia (AML) admitted to the ICU have high in-hospital mortality, ranging from 40-70% (Halpern A, JAMA Oncology, 2017, 3; 374 and Thakkar SG, Cancer, 2008, 112; 2233). A model that considers AML-specific as well as ICU-specific variables could be of great value to identify critically ill patients likely to survive beyond hospital discharge and would help providers frame goals of care discussions. The AML Composite Model (AML-CM) was recently developed to predict early as well as late mortality after diagnosis of AML (Sorror ML, JAMA Oncology, 2017, 3:1675). The AML-CM incorporates AML cytogenetic risk, age, and comorbidity burden. It is unknown whether the AML-CM scores calculated at diagnosis of AML could add prognostic value to variables collected at the time of admission to ICU. To this end, we investigated the predictive value of AML-CM scores at diagnosis in addition to other risk factors including traditional ICU markers of illness severity collected from the time of ICU admission for prediction of 90-day mortality in patients with AML.
Methods:
This is a retrospective study of 218 patients with AML admitted to an ICU at one of two affiliated referral hospitals at any time during or after the initiation of chemotherapy between 2008 and 2017. We used factors from three time points: 1) initial diagnosis: sex, race, and AML-CM; 2) time of ICU admission: age, presence of relapsed or refractory disease, history of hematopoietic stem cell transplant (HCT), presence of neutropenia with ANC<500; and 3) within 24 hours of ICU admission: highest creatinine ≥2.0 mg/dl, presence of bacteremia, use of invasive mechanical ventilation (IMV), noninvasive positive pressure ventilation (NPPV), dialysis, inotropes, and vasopressors. AML-CM was dichotomized based on a median score of 7 in our population, creating high-risk and standard-risk groups. The primary outcome was survival to 90 days after ICU admission. Risks for 90-day mortality were compared using unadjusted logistic regression, and the area under the receiver-operator curve (AUC) was calculated. Variables with p-value of less than 0.05 in association with 90-day mortality in a univariate logistic regression model were tested in a multivariable logistic regression model. Lastly, mortality at 90 days was calculated for patients with 0, 1, 2, or ≥3 risk factors for mortality.
Results:
The final study population was 217 patients, because one patient was lost to follow-up. The median age at ICU admission was 59 (range 19-83), 58% were male, and 79% were white. Mortality was 52% at 90 days. The median AML-CM was 7 (interquartile range 5-10), with 54% having AML-CM ≥7, and 46% having AML-CM <7.
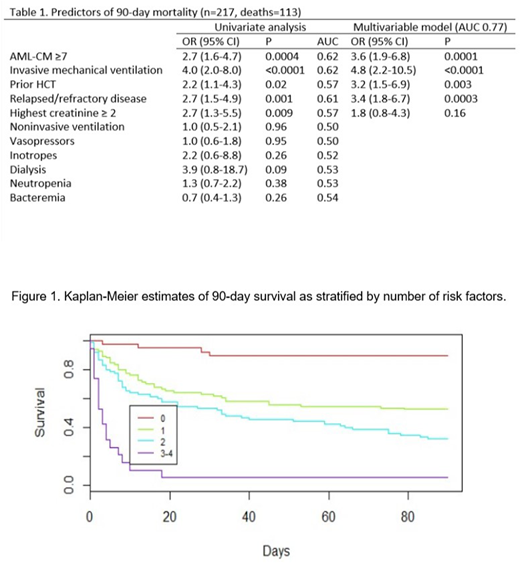
The results of the univariate and multivariable analyses are listed in Table 1. The following variables were independently associated with 90-day mortality in the multivariate analysis: AML-CM ≥ 7 was associated with 3.6 times the odds of dying (95% CI 1.9-6.8, p=0.0001); IMV, 4.8 times the odds of dying (95% CI 2.2-10.5, p<0.0001); prior HCT, 3.2 times the odds of dying (95% CI 1.5-6.9, p=0.003); and relapsed or refractory disease, 3.4 times the odds of dying (95% CI 1.8-6.7, p=0.0003).
The AUC of the multivariable model which combined the 5 variables with statistically significant association on univariate analysis was 0.77.
Based on results above, we calculated 90-day mortality rates among patients with 0 (n=39), 1 (n=84), 2 (n=75), and 3-4 (n=19) of the following factors: AML-CM ≥7, history of HCT, relapsed or resistant/refractory disease at ICU admission, and use of IMV (figure 1). Mortality rates at 90 days were 10%, 48%, 68%, and 95%, respectively.
Conclusions:
We identified 4 risk factors that show promise in predicting 90-day mortality after ICU admission in patients with AML: the AML-CM from time of diagnosis, history of HCT prior to ICU admission, disease status at ICU admission, and use of invasive mechanical ventilation within 24 hours of admission. Collectively, these factors can provide strong rationale to consider futility of ICU care among those with 3-4 risk factors, who represent ~9% of the population and have an extremely high risk of mortality at 90 days. Further, patients with 1-2 risk factors (73% of population) could be good candidates for early palliative care consult coincident with ICU admission given relatively high mortality risk within 90 days.
Becker:GlycoMimetics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal